[Presentation of Case]
A 79-year-old woman presented to the geriatrics clinic with dysuria and general weakness for 1 week. She had a medical history of hypertension, aortic regurgitation, osteoporosis with L4 vertebral compression fracture, and depression. She kept regular follow-up at our geriatrics outpatient department (OPD).
She had been in her usual state of health until 1-2 months before this admission, when increasing drowsiness and decline of physical function were noted by the family members. Two weeks before this admission, she developed numbness sensation over the four extremities and pain from the bilateral buttocks to the thigh One week prior to this admission, she presented to our geriatrics OPD with dysuria, nocturia, productive cough, general malaise, and poor appetite. She did not reported headaches, rhinorrhea, sore throat, dyspnea, abdominal pain, or gross hematuria. She appeared in acute illness and had repeated nausea and vomiting at that time. A diagnosis of acute delirium from urinary tract infection was made and she was admitted to our geriatric ward. On arrival, the blood pressure was 138/88 mmHg, the pulse rate 105 beats per minute, the respirations 18 breaths per minute, and the temperature 37.7℃. On examination, no percussion tenderness at the costovertebral angle was noted. Neurological examination showed drowsy consciousness with muscle power approximately 3/5 at the four limbs. We were not able to perform gait assessment due to general weakness. Easy choking was also noted on cranial nerve examination. The urine output also decreased to nearly zero on the same day, and the urinalysis revealed mild pyuria (WBC 10-20/HPF) and a test for nitrite was negative. Other laboratory results were shown below:
[Laboratory Study]
1.Biochemistry Data
|
4/14 |
4/17 |
4/20 |
4/23 |
4/26 |
4/27 |
4/29 |
5/06 |
Alb (g/dL) |
2.7 |
3.0 |
|
|
|
|
|
2.7 |
T-BIL (mg/dL) |
0.45 |
0.62 |
|
|
|
|
|
0.71 |
AST (U/L) |
81 |
148 |
127 |
71 |
63 |
|
77 |
127 |
ALT (U/L) |
70 |
90 |
80 |
60 |
42 |
|
51 |
67 |
ALP (U/L) |
63 |
|
|
|
|
|
|
252 |
GGT (U/L) |
183 |
206 |
|
|
|
|
|
330 |
UN (mg/dL) |
75.4 |
93.1 |
69.9 |
71.8 |
78.7 |
70.6 |
59.5 |
53.6 |
CRE(mg/dL) |
2.0 |
2.4 |
2.2 |
2.6 |
2.6 |
2.0 |
1.7 |
2.4 |
Na (mmol/L) |
131 |
140 |
134 |
134 |
133 |
134 |
137 |
131 |
K (mmol/L) |
4.2 |
3.1 |
4.0 |
3.3 |
2.5 |
3.1 |
3.5 |
3.7 |
CRP (mg/dL) |
1.26 |
|
|
|
|
|
|
0.72 |
2.Hemogram
|
4/14 |
4/17 |
4/20 |
4/23 |
4/26 |
4/29 |
5/06 |
5/09 |
Hb (g/dL) |
9.7 |
10.4 |
8.9 |
8.3 |
8.8 |
9.6 |
10.5 |
9.4 |
MCV (fL) |
85.4 |
85.4 |
88.0 |
82.2 |
80.5 |
80.7 |
82.8 |
82.8 |
PLT (K/μL) |
169 |
206 |
174 |
168 |
159 |
152 |
150 |
145 |
WBC (K/μL) |
11.53 |
7.66 |
10.00 |
7.21 |
7.57 |
7.55 |
5.76 |
7.55 |
Band (%) |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.9 |
2.0 |
1.9 |
Seg (%) |
86.0 |
82.9 |
75.7 |
81.9 |
74.5 |
81.3 |
52.0 |
78.1 |
Eos.(%) |
0.3 |
0.3 |
1.1 |
0.9 |
0.0 |
0.9 |
1.0 |
0.0 |
Baso.(%) |
0.3 |
0.1 |
0.4 |
0.0 |
1.9 |
0.0 |
2.0 |
0.9 |
Lym.(%) |
9.6 |
12.4 |
18.7 |
12.4 |
15.1 |
8.4 |
21.0 |
7.6 |
3.Coagulation Profiles
|
4/14 |
4/17 |
4/19 |
5/13 |
PT (sec) |
33.6 |
14.0 |
12.5 |
10.7 |
PT Cont (sec) |
11.4 |
11.1 |
11.0 |
11.0 |
PT INR (*) |
3.40 |
1.35 |
1.19 |
1.01 |
PTT (sec) |
|
32.0 |
28.7 |
34.5 |
4.CSF study
|
2013/04/19 |
RBC |
2 |
WBC |
0 |
TP (mg/dL) |
160.7 |
LDH (U/L) |
100 |
Glucose (mg/dL) |
<10 |
CSF Cytology |
Negative for malignant cells.
Cryptococcus-like organism identified. |
Gram's stain |
Negative |
India Ink smear |
positive |
Serum cryptococcal Ag test: positive ( > 1:512)
CSF cryptococcal Ag test: positive ( > 1:512)
CSF fungus culture: Cryptococcus neoformans
Blood culture: Cryptococcus neoformans
CSF viral isolation: negative. CSF bacterial culture: no growth.
5.Serology and Virolog
|
CEA
(ng/mL) |
CA-125
(u/ml) |
CA 15-3
(U/mL) |
CA-199
(U/mL) |
SCC
(ng/ml) |
5/28 |
19.05 |
259.4 |
19.2 |
129.65 |
76.8 |
|
HBsAg
(IU/ml) |
HBeAg |
AFP
(ng/mL) |
HCV viral load
(IU/mL) |
Anti-HIV |
Anti-HCV Ab |
4/15 |
Negative |
Negative |
7.67 |
|
|
Positive |
5/9 |
|
|
|
83000 |
Negative |
|
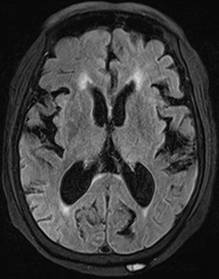
6.Brain MRI:
[Course and Treatment]
Cefuroxime was administered vein for suspected urinary tract infection. A urinary catheter was placed to relieve urine retention. She received opioid analgesics for relief of numbness and soreness from the buttocks to the thighs. Straight- leg raising test showed negative findings. Motor and Sensory nerve conduction velocity tests showed sensorimotor polyneuropathy. The results of the laboratory tests revealed ALT 114 U/L, creatinine 2.1 mg/dL, and prolonged PT (33.6 sec), and positive anti-HCV. The abdominal sonography showed liver cirrhosis. Acute kidney injury on chronic kidney disease was suspected, and adequate hydration was given. She denied food intake and medications, and a nasopharyngeal tube was inserted. Drowsy consciousness and seizures twice with right deviation of the gaze for several minutes occurred on the 4th hospital day. Computed tomography ( CT) of the brain showed brain atrophy without intracerebral hemorrhage, but the electroencephalography revealed moderate to severe diffuse cortical dysfunction. The serum electrolytes levels and hemogram were within normal limits. Tonic seizures with upward gaze nystagmus and loss of consciousness were noted twice on the 7th hospital day. Intravenous lorazepam and antiepileptics were administered. The magnetic resonance imaging (MRI) for brain showed leptomeningeal process, for which lumbar puncture was performed for suspected meningitis. The open pressure was 335 mmH2O. India-ink smear of a cerebrospinal fluid (CSF) specimen yielded a positive result for cryptococci, and total protein was elevated (160.7 mg/dL). A diagnosis of cryptococcal meningitis was made, and flucytosine and liposomal amphotericin B were given. Lumbar puncture was repeated to relieve increased intracranial pressure. Tests for cryptococcal antigen of CSF and blood specimens were elevated. Cultures of CSF and blood specimens both yielded Cryptococcus neoformans. She was transferred to infectious disease ward. Hypokalemia developed during the treatment course, for which intravenous potassium chloride was given. Due to poorly controlled high incracranial pressure, a lumbar drainage tube was placed, followed by placement of an extra-ventricular drain (EVD). After CSF cultures yielded no growth of cryptococcus, liposomal amphotericin B and flucytosine were switched to fluconazole. The consciousness level fluctuated. Tumor markers survey revealed elevated CEA (19.05 ng/mL), CA-125 (259.4 U/mL), CA-199 (129.65 U/mL), and SCC (76.8 ng/mL), but further tumor work-up was denied by the family due to the old age of the patient. The patient expired when she subsequently developed healthcare associated pneumonia.
在老年病患發生意識改變、活力變差或功能退化等情況,應從多面向去思考各種可能的原因,尤其老年病患的感染症常會以非典型的症狀來表現,因此更需要去提高警覺,以及早診斷。一些慢性感染的病原體,諸如真菌、結核菌、非結合分枝桿菌及寄生蟲等,都不太容易在感染的初期就診斷出來。
新型隱球菌(Cryptococcus neoformans)是一種酵母菌型(yeast-like)的真菌,其形狀為球型,並有莢膜(capsule)包被。它在自然界中,主要分佈於鳥類的排泄物及土壤中,尤其是鴿子的排泄物。其在臨床上可以造成各式各樣不同的疾病,最常侵犯到肺部及腦部,也可造成皮膚、軟組織、腸胃道、泌尿道及頭頸部的感染。隱球菌雖然可以在免疫力正常的宿主造成感染,但卻鮮少造成臨床上顯著的疾病。它主要對於免疫力有缺陷的宿主,會造成較嚴重的疾病,常見免疫力缺損的宿主包括:糖尿病患、血液腫瘤疾病患者、器官移植後需服用免疫抑制劑的病人、需長期使用類固醇的患者,及人類免疫缺乏病毒 (human immunodeficiency virus, HIV)感染且血液CD4 T淋巴球數量小於200/μL者。而老年人則是一群易被忽略潛在有免疫功能缺損的族群。近年來由於HIV在世界上的流行,也使得隱球菌症(cryptococcosis)的患者跟著多了起來,但隨著組合式抗病毒療法(combinational antiretroviral therapy, cART)廣泛使用,HIV感染者身上的病毒量得到控制,CD4 T淋巴球數量回升,也使其發生隱球菌症的機率下降。但在我們提出的這個病案,並沒有如上所述這些明顯的免疫缺損狀態,因此高齡應是其較易感染的原因。
隱球菌症可發生於全世界各地,尤其在熱帶、亞熱帶是主要的流行地區。每年全球約有將近一百萬人發生隱球菌症,並造成每年大於六十萬人的死亡。台灣於北迴歸線以北的亞熱帶是主要的流行區之一。
在致病機轉方面,人類由環境中接觸到潛藏新型隱球菌的生物或物質之後,會從肺部吸入隱球菌孢子或細胞,進到肺泡後嵌入肺泡細胞並潛伏於巨噬細胞,造成肺部隱球菌症(pulmonary cryptococcosis)。在第二階段,這些潛伏的隱球菌會進入血液或淋巴,可表現出隱球菌血症(cryptococcemia)或瀰漫性隱球菌症(disseminated cryptococcosis),它也可穿透血腦障蔽(blood-brain barrier)到達中樞神經系統造成隱球菌腦膜腦炎或腦膜炎,嚴重者甚至會產生隱球菌瘤(cryptococcoma)。
關於老年病患的隱球菌腦膜炎,曾祥洸醫師等人在2007年的台灣老年醫學雜誌中有分享一篇在北部某醫學中心所做的回溯性研究,其收集從1992年至2006年期間的隱球菌腦膜炎病案共39例進行分析,發現老年病患感染隱球菌腦膜炎特色包含: 女性患病比例較高;較常出現發燒、頭暈、步態不穩、嗜睡、意識改變;較少出現頸部僵硬或頸部酸痛。另外,老年病患頭痛比率不高,有可能是因為腦壓昇高或水腦的比率不高的關係。
由於隱球菌腦膜炎常造成腦壓過高,因此利用腰椎穿刺抽取腦脊髓液進行檢查並測量腦壓,是非常重要的。不過在一些意識不清或有局部神經學症狀的患者,必須先做電腦斷層或磁振造影檢查排除可能的實質腦病變或腦壓過高的狀況,避免貿然進行腰椎穿刺,而導致腦疝脫(brain herniation)的情形。當發現患者的腦壓高於250 mmH2O,反覆的腰椎穿刺來降壓至小於200 mmH2O或降壓50%,對於神經學預後是有幫助的,有時需要一日一次或多次的穿刺才能達到較好的降壓效果,甚至須提早會診神經外科醫師介入評估,是否須放置腰椎引流管或腦室外引流管來進行頻繁的引流。
在診斷方面,如果在無菌部位發現隱球菌菌體,可做為診斷依據。在腦脊髓液,用India ink染色法可觀察到隱球菌細胞的莢膜,因為它的莢膜會排開染劑的顆粒,使菌體顯現出來;但在菌量較少的病人,可能會有染不出來的情形。血液及腦脊髓液如果培養隱球菌陽性,是診斷的依據之一。對於隱球菌腦膜炎患者,腦脊髓液檢查可見到單核細胞增多及蛋白質含量上升的情況;血液及腦脊髓液的隱球菌抗原偵測(cryptococcal antigen)更是有用的診斷工具,具有不錯的敏感性及特異性。但隱球菌抗原檢查在肺部隱球菌症常呈現陰性,因此其在肺部感染的診斷用途就比較有侷限性。
針對隱球菌症的藥物治療,可依其不同的感染範圍來作探討。對於輕至中度單純肺部感染且沒有侵犯腦部者,可用fluconazole一天400 mg治療六至十二個月。對於嚴重感染者或是有侵犯中樞神經系統的病人,治療會分成三個階段,首先是誘導治療(induction therapy),可使用amphotericin B deoxycholate每日0.7-1.0 mg/kg加上flucytosine每日100 mg/kg(分四次給予),治療至少兩週至腦脊髓液培養陰轉之後,再進入鞏固治療(consolidation therapy),以fluconazole每日200-400 mg治療六至十二個月;在一些免疫力低下的宿主(如:HIV感染者且CD4 T淋巴球小於200/μL),則要進行維持治療(maintenance therapy),口服fluconazole每日200 mg,直到免疫力回升為止。由於amphotericin B deoxycholate有腎毒性、電解質失衡、發抖、發燒等副作用,所以在腎功能不全的病患(如本案例),不太適合使用,而可考慮以脂質體劑型的amphotericin B來替代進行治療,如用liposomal amphotericin B每日3-4 mg/kg來進行注射治療。
總而言之,老年病患的感染症常會有較不典型的表現,因此在臨床上對於老年病患的整體評估要更加詳細,以能及早對可能潛在的感染,做出正確的診斷,而達到早期治療的目標。對於我們提出的這個病案,在一開始觀察到病人有近期認知功能上新的變化時,就可能要懷疑有中樞神經系統的實質病變,要及早進行相關影像學檢查,搭配病史詢問,詳細地釐清可能的旅遊及接觸史(這位個案後來發現先前有禽鳥接觸史),去想到可能有隱球菌感染的可能性,在進行腰椎穿刺之前,可先做隱球菌血清抗原檢查,或許可更早獲得診斷線索,以盡速確立診斷。
參考文獻
1. 曾祥洸等。台灣老年醫學雜誌。2007;3:12-24.
2. Perfect JR, Dismukes WE., Dromer F, et al. Guidelines for management of cryptococcosis. Clin Infect Dis. 2010;50:291-322.
3. Govender NP, Meintjes G, Bicanic T, et al. Guideline for the prevention, diagnosisand management of cryptococcal meningitis among HIV-infected persons: 2013 update. S Afr J HIV Med. 2013;14:76-86.
4. Perfect JR. [title?]. In: Mandell Douglas and Bennett's Principles and Practice of Infectious Diseases. 7th ed. Chapter 263: 3287-3303.
|